Click to download
Protect Mental Health Care Coverage
What’s Happening
Wit v. United Behavioral Health (UBH) is a class action suit involving over 50,000 plaintiffs and UBH — a subsidiary of United HealthCare, the nation’s largest insurer. In an original 2019 decision, the U.S. District Court for Northern California found that UBH created flawed medical necessity criteria for determining whether to cover mental health and addiction treatment that were based on its own financial interests rather than accepted clinical standards.
However, in March 2022, a 3-judge panel at the appellate court reversed this ruling. The 3-judge panel’s decision permits the largest insurer in the country to put its own financial interests ahead of patients – and sets a dangerous example for how other insurers can limit coverage of urgently needed mental health and addiction treatment. The ripple effects of a Wit ruling impact the healthcare of over 130 million Americans.
Get Out the Message
How You Can Help
In the next few weeks, 9th Circuit judges will decide whether they will hear an appeal to en banc review for Wit. We’ve created several click to tweet links and newsletter copy below to help you easily share the message and create some noise about the importance of reviewing this case. The messages explain the case, highlight the importance of this landmark moment, and outline the opportunity at hand. Feel free to adapt to your own voice or use it as is.
We’ve also developed a number of graphics to supplement your sharing and accompany the social and newsletter copy. You can find these graphics and links to download them at the end of the toolkit.
General Awareness: click to tweet
| We stand with clinical experts, health advocates, & 50,000 plaintiffs fighting for mental health and addiction support as insurers deny coverage for care.
We can’t allow insurers to prioritize profits over people during a mental health crisis: https://www.thekennedyforum.org/wit/ |
Awareness – The Issue: click to tweet
| Who should be making decisions about mental health and addiction coverage — clinicians or insurers?
The answer should be obvious, but the current Wit v. United Behavioral Health ruling allows insurers to prioritize profits over treatment: https://www.thekennedyforum.org/wit/ |
Awareness – Urgency: click to tweet
| One of the most significant health policy cases of the 21st century is before the 9th Circuit right now. The ripple effects of this case will impact over 130 million Americans’ health coverage.
Keep your eye on Wit v. United Behavioral Health: https://www.thekennedyforum.org/wit/ |
Awareness – Profits: click to tweet
| People > Profits
Our guardrails for effectively treating mental health and addiction are under threat. We can’t let insurers prioritize profit rather than the interests of people seeking treatment. Learn more about Wit v. UBH: https://www.thekennedyforum.org/wit/ |
Awareness – Rehearing: click to tweet
| There’s no reason insurers should not be covering mental health and addiction treatment — especially when we’re in an unprecedented mental health and addiction crisis.
It is essential to revisit Wit v. UBH if we’re going to make progress: https://www.thekennedyforum.org/wit/ |
Impacts – Cost: click to tweet
| Nearly half of the 5.8 million adults with mental illness went without needed services because of cost.
Unless the court takes action, even more will be affected. Learn about this landmark case: https://www.thekennedyforum.org/wit/ |
Impact – Access to Mental Health Care: click to tweet
| Mental health care is a medical necessity, but over 16 million US adults don’t receive the mental health services they need.
Holding insurers accountable could change that. Wit v. United Behavioral Health must be reheard: https://www.thekennedyforum.org/wit/ |
Impact – Access to Addiction Care: click to tweet
| Substance Use Disorder care is a medical necessity, but over 16 million US adults don’t receive the addiction treatment they need.
Holding insurers accountable could change that. Wit v. United Behavioral Health must be reheard: https://www.thekennedyforum.org/wit/ |
Clinical Standards: click to tweet
| Insurers’ guidelines ≠ Medical guidelines
A 3-judge panel ruling in Wit v. UBH is setting a harmful precedent. We must hold insurers to accepted clinical standards established by medical guidelines, not insurers’ own financial gain: https://www.thekennedyforum.org/wit/ |
The Kennedy Forum- Post 1: click to tweet
Coverage for mental health and addiction treatment are on the line for millions of Americans in the reversal of the landmark ruling of #WitvUBH.
Learn more about efforts to urge the Ninth Circuit to rehear the case: https://www.thekennedyforum.org/wit/
The Kennedy Forum- Post 2: click to tweet
As we face a national mental health and addiction crisis, an en banc review of #WitvUBH is essential. Help us spread the word: https://www.thekennedyforum.org/wit/
The Kennedy Forum- Post 3: click to tweet
The outcome of #WitvUBH determines whether 130 million Americans will have access to necessary mental health and addiction treatment.
Help us urge the court to make care accessible: https://www.thekennedyforum.org/wit/
Daily Journal- Post 1: click to tweet
The Ninth Circuit Court of Appeals panel threatens to remove access to mental health and substance use treatment for millions of Americans in the case of #WitvUBH.
Find out why the court must grant the petition for rehearing: https://bit.ly/3H4kUZ8
Daily Journal- Post 2: click to tweet
If the Ninth Circuit panel decision in #WitvUBH stands, it will endanger mental health and addiction coverage. A rehearing of the case is necessary to protect Americans’ access to care: https://bit.ly/3H4kUZ8
Daily Journal- Post 3: click to tweet
Despite 1 in 5 adults in the U.S. living with a mental health condition, the Ninth Circuit Court ruling in #WitvUBH would endanger access to care unless the petition for rehearing is granted: https://bit.ly/3H4kUZ8
Anchorage Daily News- Post 1: click to tweet
Access to mental health services are critical for all Americans, including 108,000 Alaskans living with mental health conditions. We strongly urge the full Ninth Circuit Court of Appeals to rehear #WitvUBH: https://bit.ly/3NWuAHa
Anchorage Daily News- Post 2: click to tweet
Alaskans’ access to mental health and addiction treatment is being threatened. The Ninth Circuit Court ruling on #WitvUBH must be reheard to protect their access to healthcare: https://bit.ly/3NWuAHa
Anchorage Daily News- Post 3: click to tweet
The current #WitvUBH ruling puts the financial interests of insurers ahead of patients’ needs. We must urge the court to rehear the case to advocate for the 108,000 Alaskans with mental health conditions and millions of Americans who need access to care: https://bit.ly/3NWuAHa
The Washington Post- Post 1: click to tweet
In the case of #WitvUBH, the Ninth Circuit Court of Appeals ruling allows the largest insurer to deny coverage for mental health and addiction treatment. The case must be reheard to prevent more families from experiencing devastating impacts: https://wapo.st/3zpd9eu
The Washington Post- Post 2: click to tweet
Max Tillitt died after being denied coverage for addiction treatment by United Behavioral Health. The court must rehear #WitvUBH to prevent insurers from putting their financial interests ahead of families: https://wapo.st/3zpd9eu
The Washington Post- Post 3: click to tweet
The pandemic has increased the demand for mental health coverage. Learn how the landmark ruling of #WitvUBH determines whether or not millions of Americans have access to care: https://wapo.st/3zpd9eu
Newsletter Copy
We stand alongside clinical experts, mental health and addiction advocates, and 50,000 plaintiffs in Wit v. United Behavioral Health (UBH) fighting to protect mental health and substance use disorder coverage. At stake in this case is whether the largest insurer in the country can put its own financial interests ahead of patients – and in the process, set a dangerous example for how other insurers can limit coverage of urgently needed mental health and addiction treatment.
The U.S. District Court for Northern California ruled in 2019 that UBH ignored accepted clinical standards to prioritize profit over people’s needs, but the ruling was recently reversed by a 3-judge panel of the 9th Circuit Court of Appeals. If left unaddressed, the panel’s ruling would establish a harmful precedent for other insurers — amidst a historic mental health and addiction crisis, no less. The ripple effects of a Wit ruling impact the healthcare of over 130 million Americans.
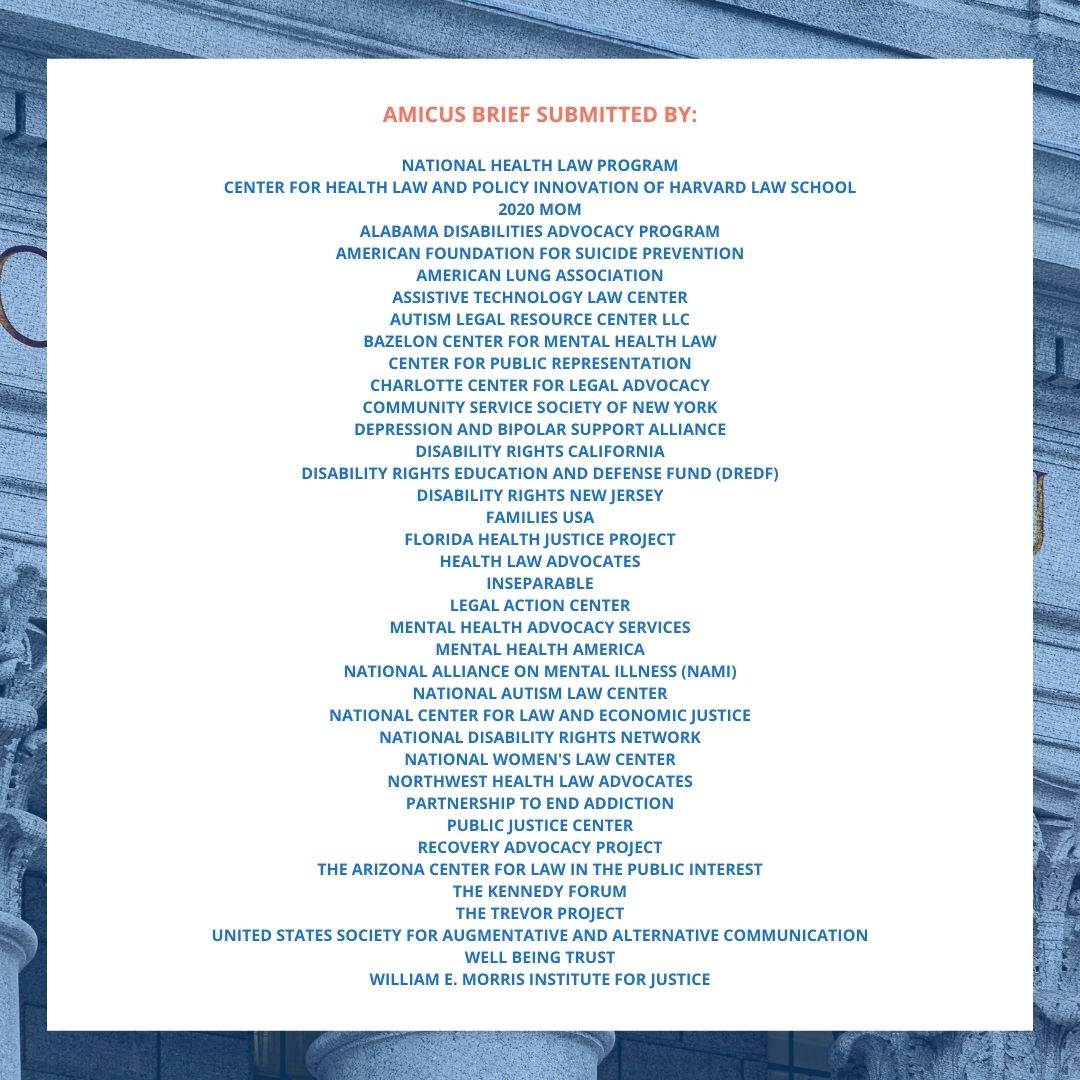
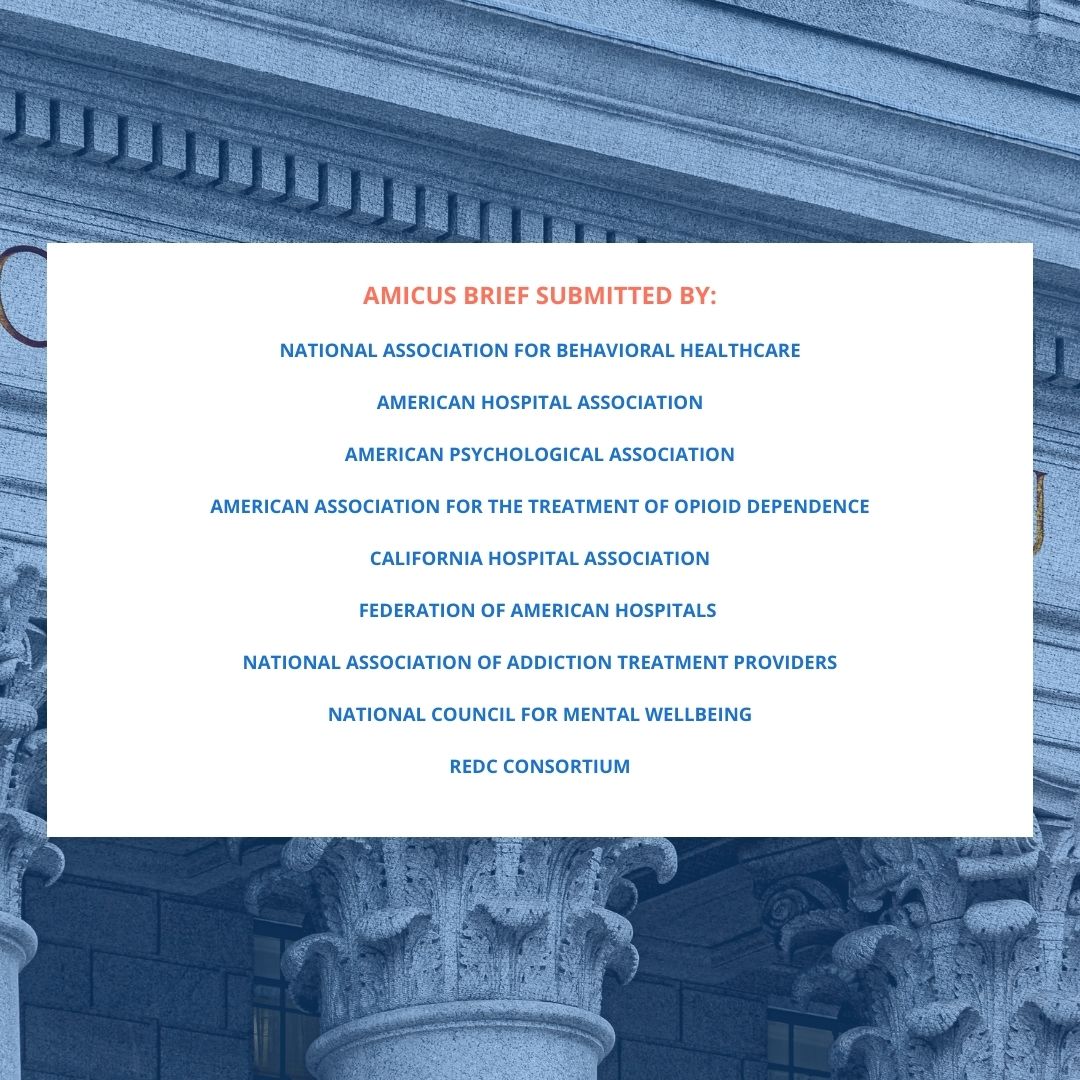
Leading mental health advocates and practitioners pushed back on the 3-judge panel ruling by filing amicus briefs that urge the 9th Circuit Court of Appeals to rehear the case, emphasizing that implications will be significant if insurers are allowed to make decisions out of step with clinical standards:
“Patients will suffer as a result [of the panel’s reversal]. When insurers are given the authority to ignore expert consensus treatment guidelines and deny authorization for covered medically necessary treatment based on financially influenced internally developed guidelines, patients are forced to forego medically necessary care. This is especially problematic in a world where so many people with behavioral illnesses already do not receive the care they need.” – National Association for Behavioral Healthcare, American Psychological Association, American Hospital Association, et al.
A rehearing from the full 9th Circuit offers an opportunity to revisit the panel’s flawed ruling, which allows insurers to deny coverage of medically necessary treatment during a historic national mental health and addiction crisis. Learn more about the case and why this is one of the most significant health policy cases of the 21st century.
Graphics
Please use the following graphics to support social media and newsletter coverage. Each set features key quotes from amicus briefs submitted earlier this week. Click on each image to download.