
Caption: Jacobson attends an event as an expert across multiple topics regarding ASD and MHPAEA advocacy.
As a mother of a children with autism spectrum disorder (ASD), Kristin Jacobson remembers times when she could only focus on getting through the next task at hand.
“I remember I watched the documentary ‘Autism, the Musical’ and there was this scene where this mom was just saying, ‘Lord, let me get through the bath,” Jacobson said. “It resonated. I would think to myself that I just need to get through whatever was next — getting in the car, getting out of the car, driving down the road.”
Beyond her challenges as a caregiver, Jacobson faced formidable impediments in accessing insurance covered health care for her kids early on.
“When we started, absolutely everything was denied care,” she said.
Jacobsons’s experiences led to decades-long work as an advocate and leader for the autism community, fighting serial rejections within the health care industry — particularly when it comes to insurance coverage issues. “A team of mostly parents-turned-advocates had to specifically legislate autism coverage in all 50 states, in all 50 Medicaid agencies, and every exchange we have it covered in.”
The first ASD treatment mandate was not until 2001, and though 46 states now have a patchwork of different mandates at varying levels, coverage remains a critical issue.
ASD is a developmental disorder that, in many health insurance plans, is categorized within mental health, which falls under the protections of The Mental Health Parity and Addiction Equity Act (MHPAEA). MHPAEA, co-authored by The Kennedy Forum co-founder Patrick J. Kennedy, ensures that coverage of mental conditions is no more restrictive than for physical conditions. Yet for autism, and many other mental health diagnoses, MHPAEA requirements aren’t typically enforced.
“All of the parity issues that come up with mental health issues kind of come up on steroids for the autism community,” Jacobson said. “What’s actually covered is as little as can be covered.”
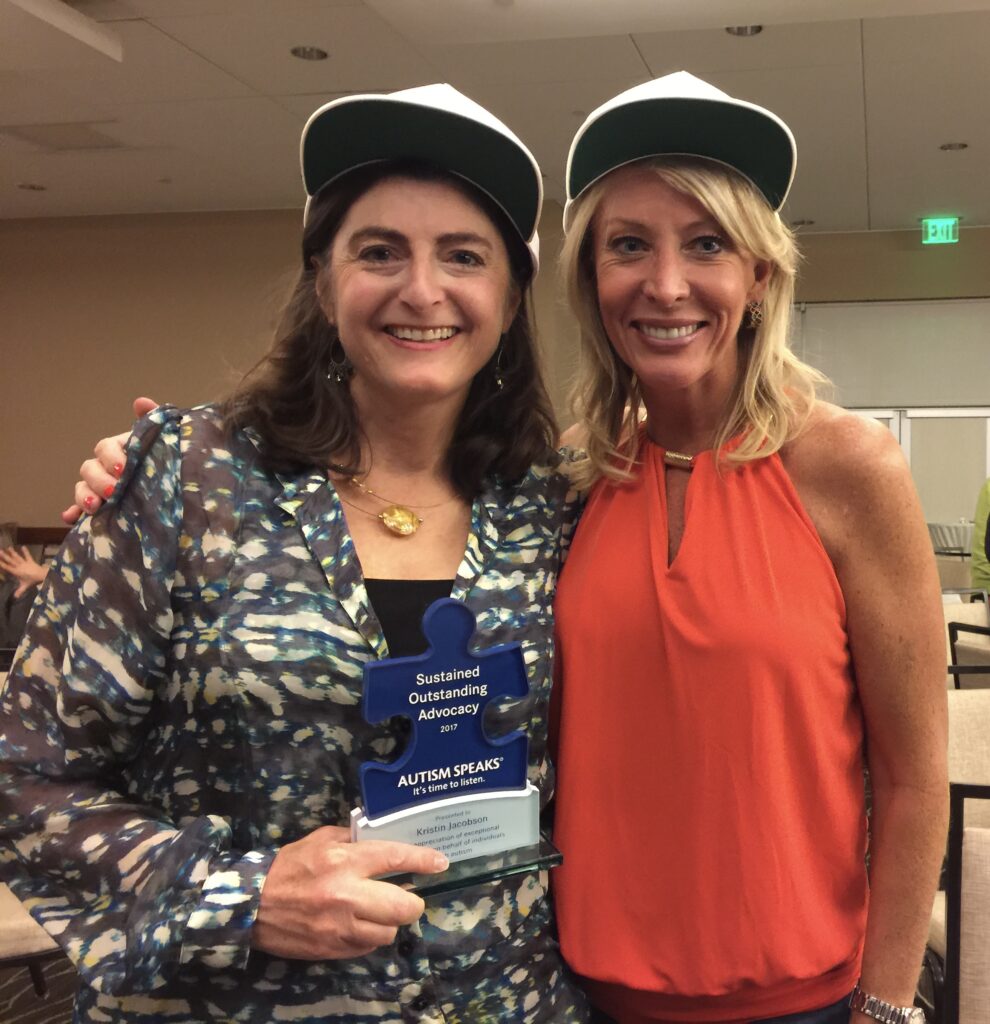
Caption: Jacobson receiving an award for outstanding advocacy from Autism Speaks.
Families Struggle to Find the Appropriate Level of Care
Some research-based intensive behavioral interventions for ASD, such as Applied Behavioral Analysis (ABA), require between 20-40 hours per week to be effective for key areas, like intellectual functioning and adaptive behavior.
This level of care is rarely covered without high scrutiny, hurdles, and limits.
“It’s one of the few conditions where it’s not standard to give the medically necessary, evidence-based dose,” Jacobson said. “You wouldn’t give half or a quarter of the dose of cancer treatment or insulin.”
Insurers sometimes deny mental health treatment based on their perception of progress — if the patient achieves too much, treatment can be deemed unnecessary; too little and the treatment is considered ineffective. For autism care, there is an added layer of complexity when considering what advancement looks like.
Jacobson recounted a story of a mother who was trying to find care for her child who had autism and seizures and could not swallow his seizure medication. Still, behavioral treatment was denied because the health plan arbitrarily determined that the patient would be unable to benefit based on his perceived cognitive ability.
Jacobson helped the family appeal the decision and eventually won. The child was able to receive treatment and was subsequently able to swallow his seizure medicine and avoid harmful monthly anesthesia, which resulted in better seizure control and improved outcomes. “Even if that child is not speaking or going to college, that is still drastically improving the quality of life — that is meaningful.”
Families caring for a loved one with ASD face compounding challenges. They must understand the diagnoses and its implications, seek out appropriate treatment, and often coordinate multiple specialist appointments, which researchers find “can profoundly alter family dynamics and interpersonal relationships,” all while trying to fight denials and delays in care.
The lack of coverage can force families to forego care altogether or cover costs out-of-pocket, leading to financial stress and insecurity.
“There were a lot of times early on when we would pay the electricity bill when they would come to shut off the electricity,” Jacobson said. “We were a missed mortgage payment away from losing the house. Though we managed to avoid that, many, many families did lose their homes.”
Caption: Jacobson and fellow advocates at an event.
Mental Health Parity Is Critical for Giving Families What They Need
Jacobson’s advocacy continues, ensuring that mental health parity is enforced so that families can find relief from cascading complications that inhibit well-being.
“I feel like I’m shouting alone from the rooftops, but I’m going to keep on shouting,” Jacobson said. “People need to understand the connection between mental health parity and the Affordable Care Act, which is arguably strongest and most widespread application of mental health parity within the insurance ecosystem. It’s the lynchpin of mental health parity.”
>>> READ MORE HERE ABOUT MENTAL HEALTH PARITY AND THE ACA
Almost 25 years after the first ASD insurance mandate, Jacobson says that families are still waiting for the health care system to catch up.
“Families need access. Families need to not have to wait. We need emergency care. We need crisis care. We need to find solutions, or we’re just left behind.”
“As a family, our outcomes are amazing, but it’s come at a high personal cost which I don’t want others to have to endure.”
Have you been denied coverage for your mental health? Please email info@thekennedyforum.org if you’d like to share your story. To learn more about improvements in mental health parity federally and in states, please follow The Kennedy Forum on LinkedIn, to see how we are advancing and defending mental health parity.

